A minimum-service strike across three public hospitals
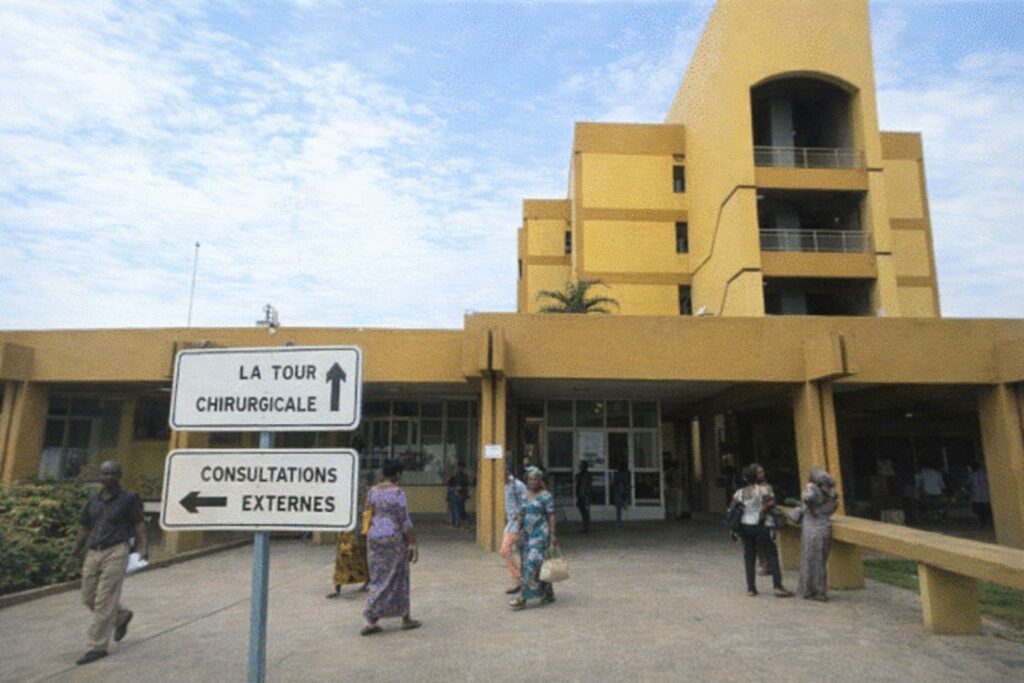
Since 24 December, staff at the Blanche Gomes Mother-and-Child Specialised Hospital, the Brazzaville University Hospital Centre, and the Djiri General Hospital have been observing an open-ended strike while maintaining a minimum level of service. According to accounts gathered at the facilities, the movement has already curtailed routine operations in multiple units, with immediate consequences for patients’ access to care.
In practical terms, the disruption has pushed some residents to turn to other health centres in the capital in order to obtain consultations or treatment that would ordinarily be delivered by these public institutions. For many families, this reorientation is not merely logistical: it can mean additional transport costs, longer waiting times, and uncertainty about continuity of care.
Paediatrics, maternity and prenatal care among the hardest hit
Several departments appear particularly affected, notably outpatient consultations, paediatric surgery, gynaecology-obstetrics and prenatal services. At the hospitals concerned, external consultations have been suspended in many cases, while admissions are reportedly limited to severe or urgent situations.
This operational configuration, combining minimum service with restricted access, tends to reshape clinical priorities. It preserves capacity for life-threatening cases but leaves a broad range of chronic follow-ups, scheduled assessments and preventive care in abeyance, a situation that can weigh heavily on maternal and child health pathways.
Patients describe cancelled appointments and growing anxiety
Patients who had travelled for scheduled appointments described a climate of disappointment and concern. One patient, who said she had come for a follow-up visit, reported that clinicians were not present at the time of her appointment, leaving her without the expected medical assessment.
Another patient, also awaiting a scheduled visit, expressed incomprehension at the situation and stressed that service users were the first to bear the consequences. Such testimonies illustrate a broader reality in periods of industrial action in essential services: the social cost is often felt most acutely by those who are already medically vulnerable.
Emergency services under pressure, with restricted access reported
In the emergency department, a death was reported at the time of a visit by observers, and access to the unit was said to have been refused. While the circumstances of the death were not detailed in the information available, the episode underscores the sensitivity of emergency care during disruptions and the need for clear protocols that protect both patients and staff.
Given the limited information, it remains prudent to avoid drawing causal links between the industrial action and any individual clinical outcome. Nonetheless, the reported restrictions on access contribute to an overall perception of tension and operational strain in critical services.
Government action expected within a framework of continuity of care
Faced with the persistence of the strike and its tangible effects on patients, calls have been voiced for public authorities to take concrete steps to restore normal functioning. In a context where health services are a cornerstone of public welfare, the priority expressed by service users is a swift, lawful and durable settlement that safeguards continuity of care.
Any resolution, to be socially credible, will likely need to reconcile staff grievances with the imperative of protecting patients’ rights to timely medical attention, particularly in high-demand domains such as maternal health, paediatrics and emergencies.